Research
OUTCOMES & IMPACTS
Converting research into socioeconomic benefits
FOOD ALLERGY
OUTCOMES & IMPACTS
To improve the quality of life of Canadians affected by food allergies, AllerGen invested $8 million to establish a translational research program focused on understanding the causes, prevalence, treatment and consequences of food allergy and anaphylaxis.
The National Food Allergy Strategic Team (NFAST)—comprising clinical, natural and social scientists working in inter-institutional teams—enabled better clinical management strategies, created innovative educational tools, and advanced policy and public health measures addressing food allergy.

With 138 refereed publications since 2007, NFAST teams and their partners across sectors have:
- produced Canada’s first food allergy prevalence data, informing Health Canada’s food allergen labelling reform initiative in 2012;
- created the first national anaphylaxis surveillance database that provides critical information on what causes anaphylaxis, how often it occurs, whom it affects, and how it is being treated across provinces;
- supported emerging clinical therapies such as food allergy oral immunotherapy (OIT) and produced new findings on the genetic basis of food allergy; and
- created innovative, award-winning educational tools, food allergy apps and peer-to-peer mentoring programs for kids with food allergies.
ASTHMA & ALLERGIES
OUTCOMES & IMPACTS
Throughout AllerGen’s 15 years as an NCE, its research teams have generated new knowledge, advanced drug development, and improved the diagnosis, management and treatment of those living and coping with asthma and allergies.

From the Clinical Investigator Collaborative (CIC) clinical trials consortium, to the Gene-Environment Interactions and Biomarkers & Bioinformatics Enabling Platforms and the CHILD Cohort Study, AllerGen-funded teams and projects have investigated the genetic, environmental and mechanistic causes of asthma and allergies and identified new therapies and approaches to treat these conditions from childhood through adulthood.
MICROBIOME
OUTCOMES & IMPACTS
AllerGen research, particularly studies from the CHILD Cohort Study, has provided insights into how the human microbiome—the universe of bacteria that live in and on our bodies—influences health and wellbeing, especially during childhood.
CHILD research has discovered that the gut microbiome can be altered by many factors, including the way a baby is born (C-section or vaginal delivery); what a baby is fed (breastmilk or formula); and whether a baby is exposed to antibiotics, furry pets or household cleaning products.
The study has also found that babies with low levels of four specific gut bacteria in their first three months of life are more likely to develop asthma.
OBESITY
OUTCOMES & IMPACTS
AllerGen research, especially from the CHILD Cohort Study, has revealed how environmental, including dietary, factors influence the risk of children becoming overweight.

CHILD research has discovered that the risk of a child becoming overweight can be influenced by many factors, including exposure to furry pets as a baby, the mother’s consumption of artificial sweeteners, and the use in the household of certain cleaning products.
BREASTFEEDING
OUTCOMES & IMPACTS
AllerGen’s CHILD Cohort Study (CHILD), one of the Network’s enduring Legacy Initiatives, has enabled hundreds of exciting discoveries about the impact of early life factors – such as mode of delivery, antibiotics, air pollution, pets, household cleaning products, sleep, screen time, food and nutrition – on child health and wellbeing.
Beginning in 2017, CHILD began reporting on the role of infant feeding and breastmilk composition in the development and prevention of asthma, allergies, obesity and diabetes.

Led by Dr. Meghan Azad, this portfolio of CHILD research has associated breastfeeding with favourable health outcomes such as:
- higher levels of beneficial gut bacteria and healthier growth patterns than babies not breastfed;
- the presence of hormones that may help prevent obesity;
- lower rates of wheezing – one of the most common reasons infants are hospitalized or receive medical care; and
- a lower risk of developing asthma later on.
COGNITIVE DEVELOPMENT & STRESS
OUTCOMES & IMPACTS
In the network’s earliest years, AllerGen research included a Mind-Body Interactions and Allergic Disease sub-program. Throughout AllerGen’s history, foci related to this thematic thread have persisted and evolved, generating numerous important findings.

Emerging from the Biomarkers and Bioinformatics Enabling Platform and the CHILD Cohort Study, AllerGen’s mind-body research findings have included insights into:
- the link between maternal fruit consumption during pregnancy and a child’s brain development;
- the effect of screentime on young children’s cognitive development and behaviour;
- the association between maternal stress and a child’s allergy risk;
- a protein in saliva that is a marker of stress susceptibility; and
- the relationship between a child’s sleep and his/her cognitive and linguistic abilities.
Canada’s first food allergy prevalence data
test
Prior to AllerGen’s investments in food allergy research, Canadian data on food allergy and anaphylaxis were sparse and based on imprecise estimates using US data.
FIRST NATIONAL SURVEY
In 2009, in partnership with Health Canada, AllerGen researchers Drs Ann Clarke (University of Calgary) and Susan Elliott (University of Waterloo) and their team completed the first national study on the prevalence, perception, and impact of food allergy in Canada.
The study, called SCAAALAR (Surveying Canadians to Assess the prevalence of common food Allergies and Attitudes toward food LAbelling and Risk), focused on five food allergens: peanuts, tree nuts, fish, shellfish, and sesame.
Among the 10,000 Canadians surveyed, roughly 7.5% – or one in 13 people – self-reported a serious allergy to one or more of these foods. The study also found that 50% of Canadian households were affected, directly or indirectly, by food allergies.
However, because the study was based on a national survey of randomly selected households, it did not fully represent minority populations considered to be especially vulnerable.
SECOND & THIRD NATIONAL SURVEYS
To bridge this gap, Drs Clarke and Elliott conducted a second national survey estimating the prevalence of food allergy among vulnerable Canadians, including those with low income, those with low education, new Canadians and individuals of Aboriginal identity.
Surveying Prevalence of Food Allergy in All Canadian Environments (SPAACE), published in 2014, concluded that Canadians with lower education and those who had immigrated to Canada within the previous 10 years had fewer food allergies than the general population.
Although immigrants were less likely to experience food allergy, the odds of their self-reporting food allergy increased by 2% with each additional year of residence in Canada.
This finding supports the “healthy immigrant” effect frequently observed in health research — that immigrants have a lower prevalence of several chronic conditions when they arrive in Canada, but their health status worsens over time, eventually converging with that of the Canadian-born population.
In 2020, the team published the results of a third nationwide study providing data on the nine foods most commonly associated with food allergies (peanut, tree nut, fish, shellfish, sesame, milk, egg, wheat and soy) and assessing changes in the prevalence of food allergy among Canadians over time.
The study, funded in part by Health Canada, found that the overall prevalence of food allergy remained relatively stable between 2010 and 2016.
PREVALENCE HIGHLIGHTS
- 6.1% of Canadians (2.1M people) have a probable food allergy: 1.7M adults and 470,000 children (0-17 yrs)
- The overall prevalence of food allergy in Canada remained relatively stable from 2010 to 2016
- Between 2011 and 2017, the rate of peanut allergy anaphylaxis in children declined in Canada
- 50% of Canadian households are affected, directly or indirectly, by food allergies
- Canadians with lower education and immigrants within 10 years of arrival have fewer food allergies than the general population
- Allergies to peanut, tree nut, and sesame are more common in children while allergies to fish and shellfish are more common in adults.
Results from all three AllerGen food allergy prevalence surveys are helping policymakers, researchers and clinicians to better understand the lived experiences of people dealing with food allergy and to identify and address gaps in education, health care and public policy related to this chronic condition.
“It is essential for Health Canada to understand food allergy prevalence in order to assess the effectiveness of its policies and programs. AllerGen research has given us that and will continue to inform our priorities well into the future.”
Dr. Sébastien La Vieille
Senior Scientific Advisor, Health Canada Food Directorate
Unique Canadian anaphylaxis surveillance database
test
In 2010, AllerGen established the Cross-Canada Anaphylaxis REgistry (C-CARE) to investigate anaphylaxis rates, triggers and management Canada-wide.
FIRST IN THE WORLD
C-CARE is the first registry in the world to track episodes of anaphylaxis prospectively.
The registry collects data from thousands of adults and children treated by EMS and in hospital emergency departments at 12 major centres in five provinces.
It provides critical information on what causes anaphylaxis, how often it occurs, whom it affects, and how it is being treated.
Led by AllerGen investigator Dr. Moshe Ben-Shoshan (McGill University Health Centre; Montreal Children’s Hospital), a growing slate of publications attests to the registry’s relevance: since 2013, Dr. Ben-Shoshan and his team have published 29 peer-reviewed papers that are quickly filling in the gaps of anaphylaxis knowledge.
C-CARE is a powerful tool that is generating critical knowledge on trends in anaphylaxis diagnosis, treatment and care to inform policies, programs and clinical care paths.
STAKEHOLDER UPTAKE
Health Canada, a C-CARE partner, is using the data to evaluate the role of health policies, particularly those related to food labelling, in the prevention of anaphylaxis in Canada.
The Canadian Association of Emergency Physicians (CAEP) and the Association des Médecins d’Urgence du Québec (AMUQ) are evaluating C-CARE findings with the goal of modifying treatment algorithms for patients presenting with anaphylaxis in the emergency department.
MOBILIZING KNOWLEDGE
To make sure knowledge from C-CARE reaches children, parents and caregivers, Dr. Ben-Shoshan and his team have launched a spin-off project called GEAR (Guidelines and Educational Programs based on an Anaphylaxis Registry).
Supported by AllerGen, GEAR is a video-based teaching tool and website to help individuals with food allergy improve their anaphylaxis knowledge and coping skills. Based on knowledge gaps identified by C-CARE, GEAR has already recruited 200 participants and is proving to be an effective teaching program.
MORE TO COME
Both C-CARE and GEAR will continue beyond 2020 to deliver new research, products and tools to improve the health and lives of Canadians living with food allergies and anaphylaxis.
C-CARE DATABASE HIGHLIGHTS
- Peanut is the most common anaphylactic trigger in children
- The overall prevalence of food allergy in Canada remained relatively stable from 2010 to 2016
- Between 2011 and 2017, the rate of peanut allergy anaphylaxis in children declined in Canada
- Anaphylaxis cases among children doubled between 2011 and 2015
- Annual incidence of recurrent anaphylaxis in children is 29%; food is the primary trigger
- 25% of anaphylactic events in children are due to accidental exposure to a known allergen
- Children with severe and milk-induced anaphylaxis have elevated levels of tryptase, an enzyme released by immune cells for up to 24 hours after the event
- Only 41% of adults and children experiencing food-induced anaphylaxis use their epinephrine autoinjector (EAI) before being treated at a hospital emergency room
Clinical practice guidelines for oral immunotherapy in Canada
test
In March 2020, AllerGen’s legacy partner the Canadian Society of Allergy and Clinical Immunology (CSACI) published new clinical guidelines for oral immunotherapy (OIT) – an emerging approach to treating food allergies.
OIT is a procedure that exposes an allergic individual to minute doses of an allergenic food, such as peanut, in a supervised medical setting. The dose is slowly increased, with the goal of desensitizing the patient’s immune system so that he/she can safely eat the food without experiencing an allergic reaction.
38 RECOMMENDATIONS
The Canadian guidelines include 38 recommendations for the responsible implementation of OIT in clinical practice and recognize the critical importance of adapting the treatment to individual patient needs and preferences.
The guidelines were published in the journal Allergy, Asthma and Clinical Immunology and represent the culmination of over two years’ work led by Drs Philippe Bégin (Sainte-Justine University Hospital Centre) and Edmond Chan (The University of British Columbia), both of whom are also AllerGen investigators.
In 2013, Dr. Bégin received AllerGen’s prestigious Emerging Clinician-Scientist Research Fellowship award, valued at $250,000. “That award was a turning point in my career,” says Dr. Bégin: “The Fellowship was the springboard to an international research opportunity at Stanford University where I worked with Dr. Kari Nadeau, one of North America’s foremost allergy experts and a leader in OIT.”
Many CSACI members as well as experts from the Institut National d’Excellence en Santé et en Services Sociaux (INESSS) contributed to the development of the guidelines, which lay the foundation for patient-centred ethical clinical practice that includes patients, caregivers and other stakeholders in the consultation and deliberation process.
Is there a safe “threshold” for those with allergies to consume peanut?
test
There is still no cure for peanut allergy. While desensitization through oral immunotherapy (OIT) is an emerging treatment, it is not yet considered the standard of care for peanut allergy, and total avoidance is the most common approach.
WHAT’S THE LIMIT?
AllerGen investigators Drs Susan Waserman and Manel Jordana (McMaster University) have conducted innovative studies on “peanut threshold responsiveness” – looking to identify a safe level of peanut that most peanut allergic individuals can consume without fear of anaphylaxis.
Using a double-blind placebo-controlled food challenge (DBPCFC), the researchers asked 23 allergic subjects to eat cookies that contained different levels of peanut protein at various times in a controlled environment.
By examining the subjects’ reaction patterns to the various dosages, Dr. Waserman hopes to identify a threshold dose that can be applied to the majority of those who have peanut allergies.
MEANINGFUL LABELLING
The concept of a threshold dose may be useful to the food industry and make food labels more meaningful, according to Dr. Waserman.
A proliferation of cautionary “may contain peanut” warnings on food labels has drastically reduced the choice of foods for allergic consumers.
Applying an established threshold dose, food labels would be required to list peanut as an ingredient only if the amount exceeded a recognized level that is tolerated by 90% of allergic individuals.
The concept of thresholds has been applied to other foods as well, and the concept of a safe threshold is in keeping with the direction being taken by other countries such as the USA, Australia, and the European Union.
Unravelling the cause of food allergy from bench to bedside
test
An AllerGen-supported research team has made significant inroads into understanding food allergy, particularly peanut allergy and anaphylaxis.
Drs Manel Jordana and Susan Waserman (McMaster University) provide an innovative approach to food allergy research by incorporating both clinical and preclinical components into their lab’s work.
MECHANISMS
Dr. Jordana leads the pre-clinical arm of the research, focusing on understanding the underlying mechanisms that disrupt the immune system.
His team has uncovered mechanisms involved in the development of sensitization or tolerance to food and identified long-lasting memory cells that are responsible for the lifelong persistence of certain food allergies in mice.
The findings can be extrapolated to explain lifelong food allergies in humans and represent an “important step in identifying memory cells as a therapeutic target with disease-transforming potential,” says Dr. Jordana.
DESENSITIZATION & THRESHOLDS
Dr. Waserman heads the lab’s clinical research, which delves into peanut desensitization (exposure to escalating doses of peanut) and establishing peanut threshold responsiveness.
Their lab’s next phase of research inquiry will focus on whether disrupting the networks of allergic antibodies and immune memory involved in allergy can reprogram the immune response against peanut to respond in a safe and sustainable manner.
The researchers believe that by “switching off” the memory of the culprit immune cell, they will be able to reprogram the allergic response, which could eventually lead to promising treatment options, as well as improved diagnosis and management.
Children should eat peanut early
test
Children who do not consume peanut during their first year of life are more likely to be allergic to peanut at age three, according to findings from AllerGen’s CHILD Cohort Study (CHILD).
NO PEANUT: HIGHER RISK
The study, published in November 2019 in The Journal of Allergy and Clinical Immunology: In Practice, found that infants who did not consume peanut in their first 12 months were more than four times as likely to have a clinical allergy to peanut by age three, compared to infants who consumed peanut before their first birthday.
The researchers also found that children not exposed to peanut by 18 months were over seven times more likely to be sensitized or exhibit a clinical allergy to peanut, compared to children who began consuming it before nine months of age.
“This tells us that if peanut is not introduced before 12 months, it should still be introduced as soon as possible,” says lead researcher Dr. Elinor Simons (University of Manitoba).
“Our findings are significant because the CHILD Cohort Study children are from the general population and most are not at high risk of peanut allergy; whereas some of the best-known studies on the timing of peanut introduction focus on children at the highest risk of developing peanut allergy.”
“We know that some parents worry about giving their infants potentially allergenic foods. This study’s findings should reassure parents, caregivers and healthcare professionals about the benefits of early peanut introduction for all children, even those at low risk for an allergy.”
BUILDING EVIDENCE
This research builds upon the previous finding from CHILD that delaying the introduction of potentially allergenic foods (such as cow’s milk products, egg and peanut) until after a baby’s first year may increase the likelihood of a food allergy later on.
Together, these CHILD discoveries support infant feeding guidelines that promote the introduction of potentially allergenic foods between four to six months of age. This represents an important shift in thinking away from avoidance of potentially allergenic foods, toward their early introduction to reduce the risk of food allergy later on.
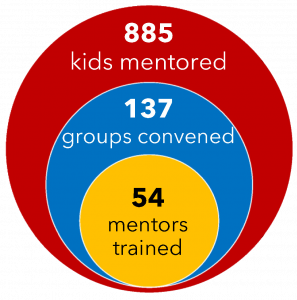
Dynamic peer-mentor program helps kids with food allergies
test
AllerGen research has been effectively translated from the academic setting to on-the-ground community organizations and into Canadian households to help kids with food allergies.
Allergy Pals is a free online program offered by AllerGen legacy partner Food Allergy Canada for children between the ages of seven and 11.
The program brings together children with food allergies and helps them develop greater confidence and coping skills by connecting them with other children and older peer mentors who have faced similar experiences. The sessions include interactive discussions, games and activities designed to promote communication, problem-solving, and support-seeking skills.
Program materials were designed by an interdisciplinary team led by AllerGen investigator Dr. Miriam Stewart (University of Alberta), with research funding provided by AllerGen. From 2011 to 2013, these resources were refined and pilot-tested with community partner organizations through grants from AllerGen and Alberta Innovates-Health Solutions.
Food Allergy Canada, one of the original project collaborators, licensed the program in 2014 to provide ongoing support to children and teens affected by life-threatening allergies. Since 2014, their Allergy Pals program has mentored over 800 Canadian kids with food allergies, held 137 groups and trained 54 mentors.
POPULAR WITH KIDS
“In program evaluations, children tell us how happy they are with the skills they have gained and the friends they have made, and nearly 100% of parents report that they would recommend the program to others,” says Kyle Dine, Food Allergy Canada’s Youth Coordinator.
Allergy Pals has grown to be so popular that in 2015, Food Allergy Canada added a new program called Allergy Allies for teens between the ages of 12 and 15. Also, because children often don’t want the sessions to end, Food Allergy Canada launched a monthly online session where new topics are introduced each month.
Asthma Canada, another AllerGen legacy partner, licensed the materials for a similar program, Asthma Pals, that was launched in 2016.
Mobile app helps kids navigate food allergy
test
Kung Food is an interactive food allergy app that is helping kids and teens navigate food allergy in a new and exciting way. Developed with AllerGen support, Kung Food is available in the Mac App Store and on Google Play.
The app aims to improve the knowledge and skills of youth living with food allergies. It features a quick reference allergy guide, an allergy attack simulator and allergy trivia games. Users test their Food Allergy IQ as they navigate through different food allergy scenarios to challenge their decision-making skills.
The app is socially integrated, allowing users to build, educate and engage their own support groups.
Kung Food was developed by nurse educators and allergists, with input from youth with food allergy, at the University of Manitoba’s Children’s Allergy & Asthma Education Centre (CAAEC). AllerGen investigator Dr. Allan Becker (University of Manitoba) led the project.
Collaborators on the project include AllerGen legacy partner Food Allergy Canada and its Youth Advisory Panel, as well as Tactica Interactive, a digital media company that specializes in cross-platform digital media strategy and products for researchers.
Making sense of food allergies
test
Theories about allergy from lifestyle “gurus” and alternative practitioners, such as homeopaths and naturopaths, have led to confusing and conflicting information to the public about the causes, triggers, and effective management of food allergies.
To help combat myths and misinformation about food allergies, an AllerGen team has produced a comprehensive, evidence-based food allergy resource guide that everyone can use.
AllerGen investigator Dr. Susan Elliott (University of Waterloo) led the creation of this unique Canadian resource with a team of food allergy researchers, physicians, stakeholder organizations and end-users.
DISPELLING MYTHS
Completed in 2020, “Making Sense of Food Allergies in Canada” is a practical, informative guide that explains the science of food allergy, the prevalence of food allergies, and the effective prevention, treatment and management of food allergies. It also dispels common food allergy myths and misinformation.
The guide will be launched to the public in 2021 through an integrated knowledge mobilization approach to support the uptake of the resource into policy and practice.
“Making Sense of Food Allergies in Canada” is adapted with permission from the UK document “Making Sense of Allergies” by the non-profit organization Sense About Science.
Paradigm shift for food allergen precautionary labelling
test
It has become commonplace for food labels to contain precautionary statements such as “may contain peanut” or “may contain traces of egg” or “made in a facility that processes milk,” whether or not a food actually contains the stated allergen.
An overuse of precautionary allergen labelling (PAL) reduces the choice of food for food-allergic consumers and raises the risk that consumers ignore a label warning altogether.
An AllerGen-funded project headed by Dr. Samuel Godefroy (Université Laval) is tackling this issue by studying the actual occurrence of allergens in foods with PALs and developing recommendations for practical labelling guidelines for food manufacturers.
The project has already produced the largest dataset ever obtained for the occurrence of food allergens in food products available for sale in Canada – in total, 3,200 food samples have been analyzed.
OVERUSE OF WARNINGS
In the first publication of the data in November 2020, in the journal Food Additives & Contaminants: Part A, the researchers found that:
- milk was detected in 23% of the samples bearing milk precautionary allergen labelling; and
- egg was detected in 7% of the samples bearing a “may contain egg” precautionary statement.
These findings confirm that most products with a PAL for milk (77%) and/or eggs (93%) do not contain detectable levels of stated allergens, suggesting the overuse of PAL by food manufacturers.
However, among the food products with a PAL for milk, chocolate products contained the highest detectable levels of milk, and were “indicative of possible health consequences if PAL was ignored by allergic consumers,” according to the authors.
The study further found that a higher proportion of products from Europe contained milk and egg allergens than products from Canada.
The project team is also evaluating the latest allergen clinical threshold data to identify a practical level of allergen (sentinel level) generally considered safe for a majority of food-allergic individuals to consume. With the allergen occurrence data and allergen clinical threshold estimates, the team will evaluate a set of risk-analysis scenarios and then form recommendations to industry on the manufacturing and labelling of foods for allergic consumers.
STAKEHOLDER ENGAGEMENT
Food allergy organizations (Food Allergy Canada, Allergies Québec), food regulatory agencies (Health Canada, Canadian Food Inspection Agency, provincial food regulators) and industry groups (food processors, retailers) have been engaged to support the development of a consensus around the proposed industry guidance.
A November 2017 meeting with 70 representatives from these groups resulted in a consensus for further action involving three streams of activity: i) defining an approach to generate and manage allergen threshold levels to support risk assessment practices and risk-based management measures; ii) enhancing guidance to industry on food allergen management; and iii) educating stakeholders on the concept of allergen thresholds and their application in risk assessment.
Additional scientific publications highlighting the project’s findings are underway. Dr. Godefroy’s team is also developing several grant proposals to seek future funding to ensure the sustainability of the project and to support final knowledge translation and communications messages to industry and consumers.
Overhauling Canada’s food labelling requirements
test
AllerGen’s investments in food allergy research and education have helped to ensure that all Canadians have access to accurate, consistent and meaningful food label information.
In 2010, AllerGen released the first Canadian food allergy prevalence data, identifying the most common food allergens among adults and children. These results helped to inform Health Canada’s overhaul of federal food labelling requirements in 2012.
GREATER CLARITY
Earlier regulations allowed manufacturers to mask some food allergens under umbrella terms such as “spices.”
The 2012 reform to the Canadian Food and Drug Regulations required the plain language declaration of allergens in food products including almonds, Brazil nuts, cashews, hazelnuts, macadamia nuts, pecans, pine nuts, pistachios, walnuts, peanuts, sesame seeds, wheat and triticale, eggs, milk, soybeans, crustaceans, shellfish, fish and mustard seed.
These changes have helped Canadians with food allergies, sensitivities and celiac disease to make more informed choices about the foods they buy and avoid accidental exposures to allergens.
The clearer language and the declaration of priority allergens, gluten sources or sulphites on labels, have also assisted new Canadians and those with lower literacy levels to easily identify foods that can be harmful, or in some cases fatal, if consumed.
Food allergy research drives library’s policy change
test
Keeping toddlers and preschoolers with food allergies safe in the busy children’s spaces of a public library can be daunting.
But the success of a “food free” pilot program – informed by AllerGen’s food allergy research – helped a Markham, Ontario library become a more welcoming space for everyone.
Markham parents Jyoti Parmar and Peter Deboran used to make regular family outings to their local library branch. But when two of their three young children developed food allergies, they began restricting their visits.
“Parents and caregivers feed children while they are playing in the kids’ book sections and story-time areas,” says Parmar. “Food drops on the floor, is smeared onto the tot tables, and even gets onto the books themselves. As parents of allergic children, we are vigilant wherever we go, but it became an enormous challenge to make sure our kids didn’t touch or eat the foods that other children were snacking on at the library.”
Citing AllerGen’s food allergy prevalence data that revealed 7.5% of the population or one in 13 Canadians has a food allergy (Soller et al., 2015), the couple made a formal presentation to the Library Board in November 2015, to share their experiences and to propose a food and beverage restriction in the children’s spaces of the library.
PILOT PROJECT PROVES POPULAR
Following a Board-approved four-month pilot project to evaluate the effectiveness and impact of a no-food zone in the children’s area, the findings were presented in May 2016.
In a customer satisfaction survey: 64% of patrons felt that the no-food zone was beneficial; 19% maintained that the library should allow food in the children’s area; and 17% had no preference.
Further, 83% reported that their satisfaction with the library had increased; 82% felt that the children’s area was cleaner; and 68% felt safer when bringing their children to the library.
As a result of the pilot’s success, the Food and Drink Policy for the Markham Public Library was amended, and all city branches adopted the no-food policy for children’s areas in 2016.
“We are excited that we can enjoy the library again as a family,” says Parmar.
“AllerGen’s research on the prevalence and impact of food allergies helped us to achieve this important change in our community, which has created a safer and more inclusive environment for the citizens of Markham.”
Evidence-based guidance on managing food allergies in childcare centres and schools
test
Managing food allergies in childcare centres and schools can be challenging and anxiety-provoking for teachers, school administrators, parents and students.
Strategies to reduce the risk of food allergic reactions across these settings have been inconsistent and increasingly become a subject of professional and public debate. For example, some people support food bans as a way to protect allergic children from accidental exposure to food allergens, while others believe bans unfairly limit food choices for non-allergic students. Some parents of food-allergic children have even taken concerns about their schools’ accommodation practices to provincial human rights tribunals.
To address these inconsistencies, an AllerGen-funded team developed a set of evidence-informed recommendations to prevent adverse reactions to food in in childcare centres and schools.
SYSTEMATIC REVIEW
Led by allergist and food allergy researcher Dr. Susan Waserman (McMaster University), the team consisted of a 22-member advisory panel, including allergy experts, community physicians and nurses, school administrators and staff, parents of allergic and non-allergic children, and leaders of community food allergy associations.
The panel conducted a systematic review of the scientific literature to collect data on the impact of select interventions – such as food restrictions, training of school personnel and stocking of epinephrine – on preventing and managing allergic reactions to food in childcare centers and schools. In addition to data on health effects, the team collected and synthesized data on the resource requirements, feasibility, and acceptability of these interventions across stakeholder groups.
“Overall, our analysis found that the magnitude of risk of a severe or fatal allergic reaction to food in childcare centers and schools was low, which is encouraging,” says Dr. Waserman.
CONDITIONAL RECOMMENDATIONS
However, the quality of available data on the impact of various interventions to reduce the risk of allergic reactions was very low. As such, the team developed “conditional recommendations” to guide best practices for food allergy management in childcare and school settings.
Conditional recommendations include:
- Implement training for teachers and other personnel in the prevention, recognition and treatment of allergic reactions to food.
- Require parents of students with a food allergy to submit an up-to-date allergy action plan.
- Implement site-wide protocols for the management of suspected allergic reactions to food in children who do not have an allergy action plan on file.
- Stock epinephrine autoinjectors (EAI) on site, rather than requiring students with a food allergy to supply their personal EAI. Allow students to carry their own EAI, if desired.
- Use epinephrine only when an anaphylactic reaction is suspected, rather than as the first universal treatment for all suspected allergic reactions.
- Do not prohibit specific foods site-wide (e.g., “peanut-free” schools).
- Do not establish allergen-restricted zones (e.g., “nut-free” classroom or “milk-free” table), however, this intervention may be appropriate in circumstances where students lack the capacity to self manage their allergen intake.
“While more research is needed, we believe these evidence-based recommendations will help to guide parents, teachers, school board officials, students and policymakers involved in discussions or decision-making about the food allergy policies of schools in their communities,” adds Dr. Waserman.
Simple urine test can diagnose childhood asthma
test
Diagnosing childhood respiratory diseases, such as asthma, bronchiolitis and obstructive sleep apnea, can be challenging. Lung function tests can be invasive and difficult to perform in young children, and there are few objective tests to differentiate respiratory conditions from one another.
With AllerGen project funding from 2007 to 2012, Dr. Darryl Adamko (University of Saskatchewan) developed a simple, non-invasive urine test for diagnosing childhood asthma in a physician’s office. The test uses “metabolomics” – the study of small molecules generated by cellular metabolism – to detect unique markers in the body that are excreted in the urine.
“When we see specific markers in the urine, they indicate tissue damage and inflammation caused by asthma,” says Dr. Adamko.
“This helps doctors diagnose asthma quickly and accurately so that treatment can begin as soon as possible to prevent further damage.”
SPIN-OFF COMPANY
With ongoing funding from AllerGen (2012-2015) and support from TEC Edmonton (University of Alberta), Dr. Adamko launched a spin-off company (Respirlyte©) in 2011 to further advance and commercialize these technologies. Using a mass spectrometry platform, Respirlyte© develops tests that identify biomarkers in the urine to diagnose airway diseases and determine severity of disease requiring therapy.
In 2013, Dr. Adamko received a $100,000 federal Grand Challenges Canada grant to further develop this technology, and in 2015, Respirlyte© was awarded $600,000 from a Western Economic Diversification Canada (WEDC) program.
“This project has the potential to change the way Canada’s doctors diagnose asthma,” said Canada’s Minister of Innovation, Science and Economic Development in a press release about the WEDC funding. “This strategic investment is one of the many ways world-class research is positioning Canada to be a global leader in science and innovation.”
WRAPPED: Improving detection of work-related asthma
test
AllerGen investigator Dr. Diane Lougheed (Queen’s University) is an expert in work-related asthma (WRA) – asthma that is caused or worsened by exposure to factors in the workplace.
As part of AllerGen’s cross-programmatic research investment in occupational and work-related allergy and asthma, Dr. Lougheed led the Network’s “WRA and Allergy Prevention and Early Detection (WRAAPED)” research program, established in 2009.
The project involved co-Principal Investigators from l’Université de Montréal, The University of Toronto, McMaster University and the University of Ottawa.
Together, the team developed a screening questionnaire to help primary care physicians recognize and diagnose WRA.
The “Work-related Asthma Screening Questionnaire Long-version”, or WRASQ(L), incorporated questions about the patient’s occupation type and duration; relationship between asthma symptoms and work; exposure to exacerbating agents such as fumes, gases, dust or other irritants; and management of personal exposures.
TOOL IDENTIFIES 40% MORE CASES
The team assessed the questionnaire’s feasibility and validity with asthma patients at outpatient clinics and an asthma education centre. The resulting tool allowed the identification of nearly 40% of additional suspected cases of WRA compared to traditional methods used in clinical practice.
The AllerGen-supported research behind the tool was published in the Journal of Asthma in September 2014. In 2015, AllerGen successfully facilitated the negotiation of a non-revenue generating licensing agreement between Dr. Lougheed and the College of Family Physicians of Ontario. Now, family physicians across the province have a reliable, efficient tool to use with patients to diagnose work-related asthma sooner.
Exposure to traffic pollution in pregnancy linked to risk of allergies
test
A mother’s exposure to traffic-related air pollution during the first three months of pregnancy is associated with an increase in her child’s risk of having allergic sensitization by age one, according to CHILD Cohort Study (CHILD) research published in the Journal of Allergy and Clinical Immunology in December 2019.
“This finding supports mounting evidence that traffic-related air pollution (TRAP) exposure in utero can be harmful and is linked to allergic sensitization, which is a risk factor for the development of asthma and allergies later in childhood,” says Dr. Stuart Turvey, senior author of the paper and Co-Director of CHILD.
The research involved mothers and their children participating in CHILD and used geospatial models of air pollution to determine the level of TRAP the mothers were exposed to during pregnancy. At one year of age, the children underwent skin prick tests to check for allergic sensitization to common food and inhaled allergens.
FIRST EVIDENCE
The study is the first to provide evidence that a biological marker known as “epigenetic gestational age” (eGA) may be used to understand how TRAP can change the molecular make-up of a cell to affect the activity of a baby’s genes related to asthma and allergy.
“We demonstrated that eGA is in the causal pathway linking air pollution to the risk of developing allergies,” explains lead author Dr. Hind Sbihi.
“We used cells from the baby’s umbilical cord to measure DNA methylation, which are biochemical marks on the DNA and its proteins.
“These marks allowed us to estimate the infant’s eGA and compare it to the infant’s actual chronological age; when there was a mismatch between the eGA and chronological age related to TRAP exposure, we found there was an increased risk for allergic sensitization.”
AirSENCE: Smart, portable air quality monitor
test
An inexpensive device developed by AllerGen researchers at The University of Toronto (U of T) provides real-time air quality monitoring that allows individuals to measure their exposure to air pollution both indoors and outdoors.
AirSENCE (Air SENsor for Chemicals in the Environment) is a portable monitor that measures the air quality health index (AQHI) and estimates concentrations of five air pollutants: nitrogen oxides, ozone, carbon monoxide, carbon dioxide and particulate matter 2.5 – one of the air pollutants most strongly linked to negative health effects.
“We began developing the prototype in 2012, as part of an AllerGen-funded research project,” says AllerGen Research Leader Dr. Jeff Brook, who co-developed AirSENCE with Network colleague Dr. Greg Evans, and former PhD student and AllerGen Highly Qualified Personnel (HQP), Dr. Natalia Mykhaylova.
“We have come a long way since our first model enclosed in a Tupperware container, and now we have different versions that can be mounted outdoors, used inside a home, or even carried.”
PILOTED IN TORONTO & BEIJING
The team piloted AirSENCE during Toronto’s 2015 Pan Am and Parapan Am Games to collect air quality information near the athletic venues. Results were posted online so that visitors to the Games – especially those with allergies, asthma or other respiratory conditions – could make decisions about when and where to train, sightsee and schedule their activities.
In addition to AllerGen support, the researchers secured financial backing from the Ontario-China Research and Innovation Fund, a program created by both governments to strengthen business ties between the two regions. Between 2016 and 2019, AirSENCE prototypes were tested at the University of Peking to evaluate pollution levels in Beijing.
AirSENCE was also used as part of the City of Toronto’s King St. pilot project – a major urban initiative that gave streetcars priority over private vehicles along a 2.6-kilometre stretch of Toronto’s King Street, the busiest surface transit route in the city.
“We installed monitors at a few selected locations in the pilot area and attached the monitor to two Toronto Transit Commission (TTC) streetcars to continuously monitor air pollution levels along the street,” says Dr. Evans.

Dr. Jeff Brook (left) and Dr. Greg Evans beside an AirSENCE monitor mounted on a street sign during Toronto’s King St. pilot project.
“The data allowed us to compare the air pollution exposure of people travelling along King Street and nearby areas, both before and after implementation of the pilot project.”
In April 2019, Toronto’s city council voted to make the King Street pilot permanent.
MAKING INFORMED DECISIONS
AirSENCE is also being employed in a number of other research projects such as measuring how much air pollution Toronto GO train and VIA train riders are exposed to, and the impact of the Kilauea eruptions in Hawaii on the air quality of villages located near the volcano.
“We are pleased that the investment AllerGen made to support our work over the years has had such an important impact in Canada and abroad,” says Dr. Brook.
“AirSENCE is empowering users worldwide to make more informed decisions about the environments they spend time in, and especially for people living with asthma and allergies, this is a huge help,” he adds.
Babies frequently exposed to cleaning products may have higher asthma risk
test
Frequent exposure to common household cleaning products can increase a child’s risk of developing asthma, according to 2020 research from the CHILD Cohort Study (CHILD).
Asthma is the most common chronic childhood disease and is the primary reason why children miss school or end up in hospital.
“In our study, we found that among the more than 2,000 babies included, those that were more frequently exposed to cleaning products in their first few months of life had a significantly higher risk for asthma and other breathing problems by age three,” says Dr. Tim Takaro (Simon Fraser University), senior author of the study.
“There is evidence linking cleaning product exposure to asthma in adults, but we believe ours is the first study to look at exposure among infants.”
Some of the prime culprits, he says, were air fresheners, plug-in deodorizers, dusting sprays, and oven cleaners.
When infants participating in CHILD were a few months old, their parents completed questionnaires about the family’s daily, weekly and monthly use of dozens of household cleaning products. CHILD research teams also visited the families’ homes to perform environmental assessments and analyze the babies’ exposure to dust, mould, and furry pets, as well as chemicals and cleaning products.
The researchers then assessed the children at three years of age to determine if they had developed asthma, wheeze or allergies.
The analyses, adjusting for other factors, found that babies with a high frequency of exposure to cleaning products had a 37% greater likelihood of being diagnosed with asthma by age three compared to babies with a low frequency of exposure.
Babies with a high frequency of exposure also had a 35% higher likelihood of developing recurrent wheezing by the same age, and a 49% greater likelihood of having both recurrent wheeze and sensitization to at least one allergen – a combination of conditions that increases the likelihood of an asthma diagnosis in later childhood.
“We found that sprayed, fragranced, and disinfecting products carried the greatest potential for harm when used at a higher frequency,” says first author Jaclyn Parks, M.Sc. (Simon Fraser University). The researchers believe that chemicals in these products can trigger the inflammatory pathways of the innate immune system, and in turn, damage the lining of the respiratory tract, which can lead to asthma and wheeze.
An unexpected finding was that exposure to cleaners impacted girls more than boys. “We’re not certain why this is but there may be some differences in immune system tuning between the genders. This question calls for more research,” says Park.
The Canadian Medical Association Journal (CMAJ) published the study in February 2020 and the researchers received over 300 requests for interviews within a few days of publication.
COVID CONSIDERATIONS
In March 2020, Dr. Takaro and Parks published a follow-up letter in CMAJ in which they acknowledged that the COVID-19 crisis “warrants the use of disinfectants at an increased frequency.”
“We remind parents that disinfectants can be used in an appropriate context and applied in a responsible manner,” they wrote, while also championing physical distancing and other measures to reduce exposure, along with frequent hand washing with soap and water and wearing masks.
Air pollution exposure in infancy and risk of allergies
test
Can breathing in traffic fumes during infancy increase the risk of allergies later on? Yes, according to research led by AllerGen investigators Drs Michael Brauer (The University of British Columbia) and Hind Sbihi (BC Ministry of Health).
Using data from over 2,400 children participating in the CHILD Cohort Study (CHILD), the team found that babies who were exposed to higher levels of traffic pollution during their first year of life were at greater risk of developing sensitivities to things like milk or peanuts, household mould, and even to cats and dogs.
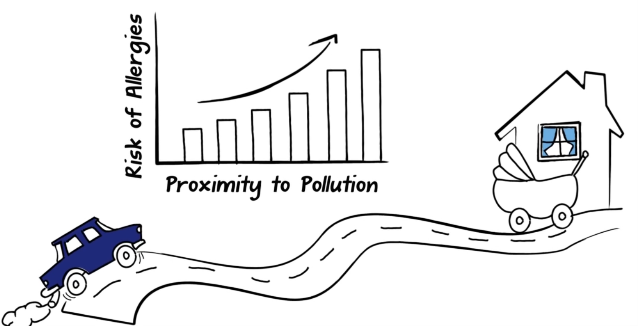
“With the increasing rates of allergies among children in Canada and elsewhere, we were interested in determining if air pollution from traffic might be partially responsible,” says Dr. Brauer.
“This was the first study to find a link between air pollution and measured allergic sensitization during the first year.”
Even a small increase in a baby’s exposure to air pollution increased the allergy risk, according to the researchers.
SIBLINGS, PETS LESSEN ALLERGY RISK
The study, published in May 2015 in the journal Environmental Health Perspectives, also found factors linked to lower allergy rates, such as owning a cat or a dog, and living in a home with no attached garage.

While infants exposed to air pollution were at greater risk, researchers did not find a link between mothers exposed to air pollution during pregnancy and allergy risk in their children. Vancouver had the largest proportion of children to develop sensitivity to allergens (23.5%), compared to Toronto and Edmonton (17% each), and Manitoba (9%).
“Understanding which environmental exposures in early life affect the development of allergies can help tailor preventative measures for children,” says first author Dr. Sbihi, who was a PhD candidate at UBC at the time.
“We also found that children who attended daycare or with older siblings in the household were less likely to develop allergic sensitization, suggesting that exposure to other children can be protective.”
Legend of Tahnee, the Wolf: asthma education for First Nations children
test
Asthma and allergies are the most common chronic conditions affecting Aboriginal children and adolescents.
In 2012-2013, AllerGen investigators completed several research studies that aimed to provide First Nations, Inuit and Métis children, families and communities with accessible, appropriate and culturally-relevant resources to help reduce the rates of asthma and allergies affecting their populations.
One of these projects, led by Dr. Dean Befus (University of Alberta) and his team at the Alberta Asthma Centre, resulted in the launch of “The Legend of Tahnee, the Wolf: My Asthma Journey” – an asthma education booklet designed by and for Aboriginal communities.
“The Legend of Tahnee” is an interactive, fun, small-group education program that optimizes asthma management behaviours, maximizes asthma control, and improves quality of life.
Program materials were adapted from the “Roaring Adventures of Puff (RAP)” child asthma curriculum developed in 1995 at the Alberta Asthma Centre. “The Legend of Tahnee” project partners included Health Canada and Asthma Canada.
LICENSED AS LEARNING TOOL
In January 2018, The Lung Association of Ontario licensed “The Legend of Tahnee, the Wolf: My Asthma Journey ©” to be used as a culturally-relevant learning tool for asthma education, awareness, and self-management across the province.
AllerGen facilitated the development of the non-exclusive, non-revenue generating license agreement between the University of Alberta and The Lung Association of Ontario through the Network’s commercialization program, which assists Network researchers to find and secure knowledge mobilization and commercialization opportunities for their research outcomes.
Since 2008, AllerGen has invested more than $1.5 million (cash) and $126,000 (in-kind) in research, and published 83 articles and presentations related to respiratory health, asthma and food allergies in Aboriginal communities. AllerGen’s partner organizations, including Asthma Canada, the Public Health Agency of Canada, Food Allergy Canada and others, have further invested over $1.8 million in cash and over $400,000 in time, expertise and non-financial resources to support these endeavours.
Half of Canadian alternative medicine clinics offer unproven asthma and allergy services
test
The majority of Canadian chiropractic, naturopathic, homeopathic and acupuncture clinics claim that they can either diagnose or treat asthma and allergies, according to an AllerGen study of nearly 400 clinic websites.
The research, published in December 2016, in BMJ Open, highlights the frequency and misleading content of marketing claims made by complementary and alternative medicine (CAM) providers in the 10 most populous cities across Canada.
AllerGen investigator Timothy Caulfield (University of Alberta), a well-known expert in health and science policy issues, led the research. Blake Murdoch, a former AllerGen Highly Qualified Personnel (HQP), was a study co-author.
UNPROVEN TESTS & TREATMENTS
“We found that alternative medicine practitioners offer a wide-range of unproven tests and treatments – everything from immunotherapy and intravenous hydrogen peroxide to ionic footbath detoxification – for asthma and allergy,” says Professor Caulfield.
“These interventions are presented to the public as legitimate; however, for the most part they are not based in science and lacked any substantial evidence of efficacy.”
For example, food-specific immunoglobulin G (IgG) testing was commonly advertised by CAM providers, despite the fact that the Canadian Society of Allergy and Clinical Immunology (CSACI), the professional association of Canadian allergists and immunologists, has recommended not to use this test due to the absence of a body of research supporting it.
More than 50% of the CAM clinics reviewed in the study made at least one health-related claim for diagnosing or treating both asthma and allergy/allergic sensitivity.
Overall, naturopath clinic websites had the highest rate of such claims: 85% of naturopath clinics claimed to be able to diagnosis or treat allergies; and 64% of naturopath clinics claimed to be able to diagnosis or treat asthma.
POLICY RESPONSE NEEDED
The study’s results highlight the need for a legal and policy response in order to protect the Canadian public from questionable claims and “to prevent the potential harm and financial exploitation of Canadians,” says Professor Caulfield.
Blood test predicts “late phase” asthmatic response
test
A blood test developed by AllerGen researchers may eventually offer a low cost, non-invasive method of predicting which individuals with asthma will develop a “late-phase” asthmatic response.
The late-phase asthmatic response is a delayed response that occurs three to four hours following an initial asthmatic reaction. About half of all people with asthma experience it – and the symptoms are usually more severe than symptoms of the initial reaction, producing mucus, inflammation, and even structural changes of the airways.
“This blood test uses NanoString© technology to look for biomarkers that indicate susceptibility to a late-phase asthmatic reaction,” says AllerGen investigator Dr. Scott Tebbutt (The University of British Columbia, PROOF Centre of Excellence).
“We hope that this test can eventually be used to identify a new target for asthma therapeutics and as a method to select patients for clinical trials.”
The technology emerged from research that Dr. Tebbutt has been pursuing with AllerGen support since 2007.
Dr. Amrit Singh (Proof Centre of Excellence), a former AllerGen trainee, is a co-author on their paper published in American Journal of Respiratory and Critical Care Medicine in February 2018.
“Our study used the test to look for differences in the blood of asthmatics who experience the late-phase response,” says Dr. Singh.
“We identified a number of molecules called RNA transcripts that strongly predicted the late-phase asthmatic response.”
FACILITATING ASTHMA DRUG DEVELOPMENT
Currently, lung function tests are the only reliable method of diagnosing a late-phase asthmatic responder.
Drs Tebbutt and Singh hope that the new technology, and the research behind it, will facilitate the recruitment of appropriate subjects for clinical trials, which, in turn, may accelerate the development of new drugs for asthma.
Biomarker to diagnose Western red cedar asthma
test
AllerGen investigators Drs Chris Carlsten and Scott Tebbutt, both at The University of British Columbia, have found a blood biomarker that can be used to diagnose an occupational asthma associated with the BC forestry industry.
For over a decade, Dr. Carlsten and his team have been diagnosing Western red cedar asthma (WRCA) at the Vancouver General Hospital.
The conventional diagnostic test takes two to three days to complete and requires that the patient inhale plicatic acid, a costly procedure that can be uncomfortable for the patient.
Plicatic acid naturally occurs in Western red cedar trees and is released into the surrounding environment when the wood is cut or milled. Exposure to the acid has led to asthma in approximately 5% of the workers who regularly inhale it.
As part of the testing procedure, Dr. Carlsten routinely collects blood samples from patients.
Collaborating with AllerGen colleague Dr. Tebbutt, he aimed to find out whether blood can be used to confirm WRCA when workers develop symptoms or when disability claims are made.
FASTER IDENTIFICATION OF THE DISEASE
Dr. Tebbutt’s team (Proof Centre of Excellence) analyzed the samples to search for patterns unique to the RNA of white blood cells from patients who tested positive during the plicatic acid inhalation test.
They found higher levels of specific RNA molecules in the blood of six of seven patients whom Dr. Carlsten had diagnosed with WRCA. These molecules are produced by two genes and, in turn, produce proteins known to affect inflammation and stress responses.
Published in the American Journal of Respiratory and Critical Care Medicine in 2017, this biomarker discovery will constitute a breakthrough for the diagnosis of WCRA, once validated by further testing with a larger sample size.
“We hope the biomarker will eventually lead to a quick and easy blood test that will make WRCA diagnosis much simpler and can facilitate identifying the disease at an earlier stage,” says Dr. Carlsten.
CIC-tested biologic hailed as “game-changing, blockbuster” asthma drug
test
From 2011 to 2013, AllerGen’s Clinical Investigator Collaborative (CIC) conducted an early Phase II clinical trial on the injectable biologic drug tezepelumab, developed by MedImmune (the biologics arm of AstraZeneca) and Amgen, and first identified the drug’s significant therapeutic potential.
Tezepelumab is an antibody that blocks the action of thymic stromal lymphopoietin (TSLP), a protein involved in various allergic diseases including asthma.
Led by AllerGen Research Leaders Drs Paul O’Byrne and Gail Gauvreau (McMaster University), the study involved researchers at five CIC sites across the country, including Dr. Louis-Philippe Boulet (Laval University); Dr. Donald Cockcroft (University of Saskatchewan); Dr. Mark FitzGerald (The University of British Columbia); Dr. Beth Davis (University of Saskatchewan); and Dr. Richard Leigh (University of Calgary).
The study found that tezepelumab successfully blocked the TSLP protein leading to a reduction in baseline inflammation and providing resistance to allergens for those with mild allergic asthma.
The findings were published in The New England Journal of Medicine (NEJM), and reported broadly in major media outlets including The Wall Street Journal and Washington Post.
In 2017, a follow-on Phase IIb trial of tezepelumab, conducted by Dr. Jonathan Corren of the University of California, Los Angeles, and colleagues, confirmed the CIC’s original evaluation and generated further expectations for an asthma treatment with “blockbuster potential.”
DRAMATIC RESULTS
“Dramatic results” from the trial were published online in the NEJM in September 2017, and presented at the European Respiratory Society (ERS) International Congress in Milan, Italy. The drug was shown to reduce asthma exacerbations in patients with moderate to severe, uncontrolled disease by between 61% and 71%, compared to placebo.
In a commentary on the findings, also published in the NEJM, Dr. Elisabeth Bel described the drug as “the broadest and most promising biologic for the treatment of persistent uncontrolled asthma to date,” positioning it as a strong contender in the multibillion-dollar market for severe asthma injections.
In November 2020, Amgen released results from a Phase 3 trial of tezepelumab, stating in its press release that the drug “demonstrated a statistically significant reduction in exacerbations compared to placebo in patients with severe asthma.”
“This is the best example to date of what the CIC can do,” comments Dr. O’Byrne. “These trial results further validate the accuracy of the CIC’s allergen inhalation challenge model and its ability to identify early those compounds, like tezepelumab, that merit continued development and those that are likely to fail in larger clinical trials.”
Since 2005, AllerGen’s CIC has conducted 29 clinical trials with 19 industry partners, attracting nearly $30 million in global pharmaceutical and biotechnology investments to Canada.
Four gut bacteria help protect kids from asthma
test
In a breakthrough finding, the CHILD Cohort Study (CHILD) has shown that four types of gut bacteria play a critical role in protecting children against asthma.
The research, published in Science Translational Medicine in September 2015, found that infants with low levels of four gut bacteria, abbreviated FLVR (Faecalibacterium, Lachnospira, Veillonella, and Rothia), at three months of age had a significantly higher risk of asthma by age three. It is the first study to establish a causal link between infant gut bacteria and the development of asthma.
CHILD Co-Director and CHILD Vancouver site leader Dr. Stuart Turvey (The University of British Columbia, BC Children’s Hospital) and CHILD investigators Dr. Brett Finlay (The University of British Columbia), and Dr. Marie-Claire Arrieta (University of Calgary) led the research.
A NEW WAY TO PREVENT ASTHMA
Most infants acquire the FLVR bacteria naturally from their environment. However, some babies are not exposed to them for various reasons, including cesarean-section delivery and exposure to antibiotics, which disrupt the normal composition of gut bacteria, the researchers said.
“This discovery is exciting because it emphasizes the importance of the gut microbiome in asthma and opens the door to a whole new way to prevent childhood asthma by supplementing these specific bacteria in the first 100 days of life,” says Dr. Turvey.
Using stool samples collected from 319 children participating in CHILD, the researchers pieced together a picture of the babies’ gut environments and the bacteria living there. They also assessed the children for early signs of allergies and asthma during clinical check-ups at one and three years of age.
Children with low levels of FLVR at three months of age were more likely to wheeze and to have positive allergy skin tests (both are telltale signs of future asthma) at the age of one year, even if their FLVR levels had normalized. The researchers confirmed the protective effect of FLVR in mice.
WORLDWIDE ATTENTION
The study quickly grabbed worldwide attention, generating over 400 headline stories within 24 hours, including TIME, The Globe and Mail, and the CBC.
The FLVR discovery opens up the possibility of identifying children most at risk for developing asthma by testing their microbiome in the first three months of life. Those children could be monitored closely and treated quickly if they showed signs of asthma. It also opens the door to developing FLVR probiotic treatments to prevent asthma in the first place.
“We received emails from families affected by asthma thanking us for this work,” says Dr. Turvey. “We believe this outpouring of gratitude attests to the burden asthma places on families. People are eager for anything that might help – even bacteria.”
Cesarean sections and other early life factors alter the infant’s microbiome
test
Events at birth may affect the microbes living in a baby’s gut during the first few months of life, leading to a higher risk of childhood obesity and allergies, according to CHILD Cohort Study research published in October 2020, in the journal Gastroenterology.
The researchers used data from 1,667 children participating in CHILD to look at the complex relationships between birth events, a baby’s gut microbiome at three and 12 months of age, and health outcomes at ages one and three.
They linked factors such as caesarean section delivery and prolonged labour to changes in the gut microbes of infants. They then determined the pathways by which these alterations may lead to an increased risk of developing allergies and obesity later in childhood.
To conduct the study, the team collected stool samples from the infants’ diapers and analyzed the samples for gut microbes and their metabolites. At one and three years of age, the children underwent skin prick tests to check for allergic sensitization to 10 common allergens.
C-SECTION BIRTH LINKED TO HIGH BMI
The researchers found that infants born by caesarean section were more likely to have a high body-mass index score at ages one and three. When the researchers examined the children’s microbiome profiles at three months of age, they found that an altered ratio of two types of bacteria – Enterobacteriaceae and Bacteroidaceae – was the dominant path to overweight.
At 12 months of age, a higher Enterobacteriaceae/Bacteroidaceae (E/B) ratio and colonization with Clostridioides difficile (C. difficile) were the main pathways leading to allergic sensitization.
Senior author Dr. Anita Kozyrskyj (University of Alberta) says the findings highlight the importance of identifying multiple and common pathways of the gut microbiome during infancy.
OPTIONS FOR PREVENTION
“Much of what happens to us later in life is related to the exposures we encounter in infancy and early childhood,” she comments.
“Understanding how disruptions to the gut microbiome affect health in later childhood means we may have several options for effective interventions to prevent these chronic conditions before they become established.”
In earlier work in 2013, Dr. Kozyrskyj published an article in the Canadian Medical Association Journal with co-author Dr. Meghan Azad (University of Manitoba), that also highlighted the potential impact of early childhood exposures, such as the method of delivery in childbirth, as well as the method of infant feeding on lifelong health.
The 2013 article went on to receive the 2014 Bruce Squires Award that is awarded annually to the “research paper published in the journal (during the previous year) that is most relevant to the practice of medicine and most likely to impact it in a positive way.”
Let Them Eat Dirt Documentary
test
In 2018, CHILD Cohort Study (CHILD) research and researchers were featured in an AllerGen-supported documentary film about the importance of early-life microbes for child health.
Specifically, the film highlights how beneficial bacteria in our bodies can be altered by our environment, promoting conditions and diseases such as obesity, diabetes, asthma, and allergies – especially among kids.
WHAT’S HARMING OUR MICROBIOME?
Based on the best scientific literature to date – including published research discoveries from CHILD – Let Them Eat Dirt: The Hunt for our Kids’ Missing Microbes connects with young families, researchers, and doctors to sleuth out what’s harming our microbiome and learn what can be done to reverse this dangerous trend.
The film features AllerGen investigators Dr. B. Brett Finlay (The University of British Columbia), a world-leading microbiologist, and microbiome expert Dr. Marie-Claire Arrieta (University of Calgary), who co-authored the 2016 bestselling book by the same name: Let Them Eat Dirt.
The film includes interviews with international microbiome experts, including AllerGen investigators, children participating in the CHILD Cohort Study, as well as parents, doctors, healthcare workers and other professionals who help explain the latest scientific discoveries and share their experiences.
Among the interviewees, CHILD co-Director Dr. Stuart Turvey (The University of British Columbia) sheds light on the link between early-life microbe exposures and long-term health, with a particular focus on asthma.
In another interview, CHILD Manitoba site co-lead Dr. Meghan Azad (University of Manitoba) explains why breastmilk should be considered the first “personalized medicine.”
The film was supported by AllerGen Strategic Initiative funding and produced by Emmy award-winning producer Rivkah Beth Medow.
Let Them Eat Dirt: The Hunt for our Kids’ Missing Microbes has been aired across Canada and is represented for distribution in the US by Bullfrog Films.

Dr. B. Brett Finlay with AllerGen President & CEO Dr. Diana Royce at the premiere screening of Let Them Eat Dirt in March 2019, Vancouver, BC.
Furry friends help fight obesity
test
Owning a cat or dog might be a good thing when it comes to reducing the risk of childhood obesity and allergies, according to 2017 findings from AllerGen’s CHILD Cohort Study (CHILD).
The research, published in April 2017 in the journal Microbiome, and highlighted in Nature Outlook, found that babies exposed to furry pets in early life had higher levels of two gut bacteria that may protect against childhood obesity and allergic disease.
AN IMMUNE SYSTEM’S BEST FRIEND
“The abundance of these two bacteria, which help to train a baby’s developing immune system, was increased twofold in babies when there was a pet in the household,” says the study’s senior author, CHILD investigator Dr. Anita Kozyrskyj (University of Alberta).
The bacteria, Ruminococcus and Oscillospira, can be passed from pets-to moms-to fetuses during pregnancy, and directly from pets to infants during the first three months of life, according to the researchers.
“We also found that the presence of pets could reduce the chances of a mother passing on a Group B Streptococcus (strep) infection during birth, which can cause pneumonia in newborns,” says Dr. Kozyrskyj.
Her team analyzed data from 746 children and their parents participating in CHILD. Information on pet ownership was reported by mothers during pregnancy and when infants were three months old. DNA sequencing techniques performed in the laboratories of CHILD researchers Drs James Scott and David Guttman (University of Toronto) provided data on the types and quantity of bacteria present in the infants’ stool.
Almost half (47%) of the children lived in households containing furry pets both during pregnancy and in the first three months of life; 45% lived in households with no pets; and 8% lived in households that contained pets only during pregnancy.
The publication was the top-scoring microbiome paper across all BioMed Central journals in 2017.

The study’s findings build on a body of evidence showing that children who grow up with dogs have lower rates of asthma, according to lead author Dr. Hein Min Tun, a former Alberta Innovates Health Solutions (AIHS) postdoctoral fellow (University of Alberta) and AllerGen Highly Qualified Personnel (HQP).
Ultimately, the CHILD team hopes that these findings will contribute to new ways of modifying the gut microbiota that can be used to prevent or treat childhood obesity and allergies.
How sweet it isn’t: What expecting moms should know about artificial sweeteners
test
In May 2016, AllerGen’s CHILD Cohort Study (CHILD) published the first human evidence that exposure to artificial sweeteners in utero influences body mass index (BMI) in the first year of life and may contribute to the development of early childhood overweight.
Dr. Meghan Azad (University of Manitoba) led the research, which was published in JAMA Pediatrics and reported around the world, including through stories in TIME, The New York Times and Cosmopolitan.
WHO’S THE BAD GUY?
“Typically, we think of sugar as the ‘bad guy,’” says Dr. Azad, who co-leads CHILD’s Manitoba site.
“It turns out that replacing sugar with artificial sweeteners in pop, or even in coffee and tea, may not be such a good idea. If a mom consumes diet drinks on a daily basis during her pregnancy, it could have an impact on her baby’s weight.”
As part of the study, over 3,000 expectant mothers participating in CHILD answered questions about what they ate and drank during pregnancy, and their babies were studied a year after birth.
Moms who reported consuming one or more artificially sweetened beverages (ASB) per day during pregnancy were twice as likely to have children that were overweight or obese at one year, compared to women who avoided these beverages.
ASB consumption in pregnancy appeared to have no effect on the infants’ weight at birth.
“This suggests that a mom’s ASB consumption likely influences her baby’s weight gain after birth, rather than during fetal growth,” says Dr. Azad.
“This association persisted whether the artificial sweeteners came from soft drinks, coffee or tea.”
WATER THE BEST OPTION
The findings do not suggest that artificial sweeteners cause obesity in children, according to Dr. Azad, but they do support previous research that found similar links between sugar substitutes and health issues, including weight gain, in animal and human studies.
Until further research provides more definitive answers, Dr. Azad advises: “When you’re pregnant, unsweetened drinks like water are likely the best option.”
Household cleaners associated with obesity in young children
test
Killing germs around the house may have an impact on young childrens’ weight. What’s the connection?
The infant gut microbiome, according to a study led by CHILD investigator Dr. Anita Kozyrskyj (University of Alberta).
Dr. Kozyrskyj’s team showed that the frequent use of household disinfectants – primarily multi-surface cleaners – may increase the risk of obesity in young children by altering the microbes in their gut.
The study, published in the Canadian Medical Association Journal (CMAJ) in September 2018, was the journal’s top paper that year for media coverage, which included Newsweek, The Globe and Mail, and CBC, and was listed by CMAJ among its “Top 25 articles of 2018.”
DOUBLE THE RISK
“We found that infants living in households where disinfectants were used at least weekly were twice as likely to have higher levels of the bacteria called Lachnospiraceae at three to four months of age,” says Dr. Kozyrskyj.
“At three years of age, those same children had a higher body mass index (BMI) than children who were not exposed to frequent home use of disinfectants as infants.”
Her research team used data from 757 children participating in CHILD and examined the effect of exposure to three categories of household cleaners – disinfectants, detergents and eco-friendly products – on the infant gut microbiome.
“We did not find a relationship between detergents and gut microbiome change or obesity risk that was independent of disinfectant usage,” she adds, noting that it was important to distinguish detergents from disinfectants since the usage of both is highly correlated.
‘ECO’ CLEANERS BETTER?
The study also found that infants in households where “eco” (or ecologically friendly) were frequently used had lower odds of becoming overweight or obese, but this was not related to their gut microbiome as an infant.
“Infants growing up in households with heavy use of eco cleaners had lower levels of different types of gut microbes such as Enterobacteriaceae. However, we found no evidence that these specific microbiome differences were associated with the reduced obesity risk,” said AllerGen Highly Qualified Personnel (HQP) Mon Tun, formerly a PhD student at the University of Alberta and first author of the study.
Tun speculated instead that mothers in households using eco products may also eat healthier food and, thus, have healthier microbiomes during pregnancy, which may in turn have a positive impact on the newborn microbiome and later weight gain.
“Our findings suggest that parents may help to protect their child’s gut microbiome and reduce the risk of weight gain and obesity by avoiding disinfectant agents in household cleaning regimes,” says Dr. Kozyrskyj.
“Bottom line: we recommend against the frequent use of disinfectant cleaners in households with infants and suggest that parents consider alternative cleaning products.”
Listen to the CMAJ podcast | Read the CMAJ commentary
Breastfeeding Outcomes & Impacts
test
Teams working within CHILD’s breastmilk research portfolio have also discovered that how a baby is breastfed matters – meaning there is a difference between feeding directly from the breast and feeding pumped breastmilk from a bottle.
Among the thousands of babies in the CHILD Cohort Study, the risk of asthma and obesity was lowest among those who received only breastmilk directly from the breast in early life.
CHILD data has also shown that breastfeeding is a strong determinant of the infant gut microbiota – the community of microbes and bacteria that live in the human digestive tract – that influences nearly every aspect of our health, from our metabolism to our immunity, and even our mood.
All of these CHILD findings are helping us to better understand the functional properties and protective effects of breast milk, which will ultimately help parents and practitioners make more informed decisions about infant nutrition.
Hear Dr. Meghan Azad talk about her breastfeeding research with the CHILD Cohort Study
“CHILD research is informing UNICEF’s efforts to advocate for better child and family policies, including improved parental leave take-up that will help mothers continue breastfeeding and keep more babies healthy.”
Lisa Wolff
Director, Policy & Research, UNICEF Canada
Benefits of “direct” breastfeeding
test
In 2017, Dr. Meghan Azad and her University of Manitoba colleague, pediatrician Dr. Annika Klopp, found direct breastfeeding for the first three months of life appears to provide more protection against childhood asthma than either infant formula or expressed breastmilk.
The research, published in The Journal of Pediatrics in November 2017, showed that the lowest risk of asthma was observed among children who were exclusively fed at the breast until three months of age.
“We expected to see a difference in asthma risk between breastmilk-fed and formula-fed infants, which we did,” says Dr. Azad.
“However, we were surprised to find that for the breastmilk-fed babies, how the babies received breastmilk seemed to matter too.”
The research analyzed data from more than 3,200 moms and babies participating in the CHILD Cohort Study (CHILD). Infants were classified into four feeding categories at three months of age: (1) breastmilk only – all direct breastfeeding; (2) breastmilk only – some expressed breastmilk; (3) infant formula and breastmilk; or (4) infant formula only. At three years of age, the children were assessed for possible or probable asthma.
LOWER ASTHMA RISK
The researchers found that asthma risk was lowest among infants who received direct breastmilk only to three months (8.8%); higher among infants receiving some expressed breastmilk (12.5%) or breastmilk and formula (14.9%); and highest among exclusively formula-fed infants (15.8%). These associations persisted after adjusting for maternal health and socioeconomic factors.
While more research is needed to explain their results, the researchers have a couple of theories.
“One possibility is that babies may develop stronger lungs through the physical act of suckling at the breast, which requires more effort than feeding from a bottle,” says Dr. Azad. “Another theory is that the steps involved in pumping and storing breastmilk might negatively affect the milk’s special cells, proteins and molecules that help to protect against asthma.”

Image from the CHILD Cohort Study breastfeeding video
Dr. Azad is quick to note that expressed breastmilk still proved more beneficial than infant formula. “Moms go through a lot of effort to pump breastmilk for their babies, and I wouldn’t want them to get the impression that it’s not worth it – there are definitely health benefits to pumped breastmilk over formula feeding.”
In January 2018, MD Magazine interviewed the researchers to help translate the findings for primary-care physicians. Dr. Azad shared with the magazine her team’s hope that the study will guide “future research on the best ways to store and feed expressed milk, and that it will inform societal policies to protect, promote and support breastfeeding.”
MD Magazine provides physicians with up-to-date specialty and disease-specific resources designed to help primary-care physicians provide better care to patients.
“Every feed counts”: Breastfeeding may protect against obesity in early life
test
Infants who are breastfed have a reduced risk of being overweight in the first year of life – and the protective association is stronger with longer and more exclusive breastfeeding, according to an October 2018 study led by Dr. Meghan Azad.
Published in the journal Pediatrics, the study looked at both body mass index (BMI) and the rate of infant weight gain – an important predictor of future obesity and cardiovascular health.
EVEN PARTIAL BREASTFEEDING IS BENEFICIAL
“We found that the risk of overweight at 12 months of age was over three times higher among infants who were not breastfed (8.3% overweight) compared with infants who were exclusively breastfed (2.4% overweight) for the first six months of life,” says Dr. Azad.
“It’s important to note that in our study, the protective effects of breastfeeding were ‘dose dependent,’ meaning that babies who were partially breastfed also received some benefit, so ‘every feed counts.’”
The study also found that the method of feeding breastmilk matters. Using data collected from more than 2,500 infants and mothers participating in CHILD, the analysis showed that babies nursed directly at the breast had a lower risk of obesity within their first year of life compared to babies who received expressed breastmilk via a bottle.
“Although, expressed milk was still beneficial for asthma risk compared to infant formula,” notes Dr. Azad.
Dr. Azad suggests that possible explanations for the differences between direct and indirect breastfeeding include: the routine steps of refrigerating and re-heating expressed milk may degrade the bioactive components of breastmilk; or infants who are fed at the breast may have better self-regulation of milk intake.

Image from the CHILD Cohort Study breastfeeding video
The findings made headlines and were picked up by international media outlets including People, CNN, Global News, CBS News, the Boston Globe, and the Chicago Tribune.
“Our hope is that this research will help to inform and optimize infant feeding guidelines, and continue to promote programs and policies that support direct breastfeeding, such as paid maternity leave,” says Dr. Azad. “Together, these measures could have a meaningful impact on preventing childhood obesity.”
Read the commentary about the study in Pediatrics.
Breastmilk sugars may help prevent food allergies
test
Specific sugars in breastmilk may help to strengthen a baby’s immune system and reduce the risk of developing food allergies later in childhood.
In addition to the simple sugar lactose, which serves as an energy source, human milk contains complex sugar molecules known as human milk oligosaccharides (HMOs).
HMOs are not digestible by infants, but they feed good bacteria in the gut, helping to shape the development of the infant gut microbiome, which previous research suggests strongly influences allergic disease.
Dr. Meghan Azad has studied the breastmilk samples collected from mothers participating in CHILD for several years, and produced exciting research findings about breastfeeding and breastmilk components.
A BENEFICIAL HMO PROFILE
“In this project, we identified a ‘beneficial’ HMO profile that was associated with a lower rate of food sensitization in children at one year of age,” says Dr. Azad.
Collaborating with co-author Dr. Lars Bode from UC San Diego, the researchers analyzed data and milk samples from 421 infants and their mothers participating in CHILD.
They found that 14% of infants were sensitized to at least one food allergen at one year of age. Although no individual HMO was associated with food sensitization, the overall HMO composition appeared to play a role in which infants developed food sensitization.
“The amount and composition of HMOs are highly variable between women, changing across different settings and populations,” says Dr. Kozeta Miliku (McMaster University), a former postdoctoral fellow in Dr. Azad’s lab and first author of the study.
“These results suggest that particular combinations of HMOs are important for infant development,” adds Dr. Miliku.
“Our hope is that this study will guide future research that may identify the maternal and environmental factors that promote a ‘beneficial’ HMO profile and that we will better understand how these bioactive molecules contribute to an infant’s developmental programming and prevention of allergic disease.”
The research was published in the journal Allergy in May 2018.
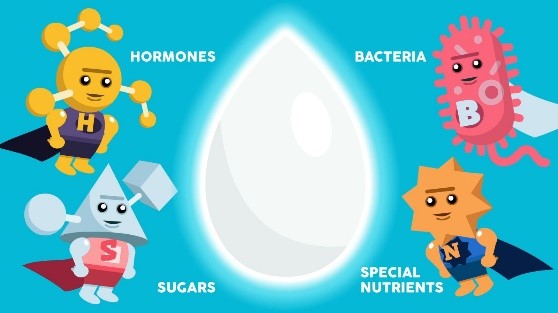
Image from the CHILD Cohort Study breastfeeding video
Breastmilk bacterial profile different when milk is pumped
test
To build on her previous breastmilk discoveries, in 2018-2019, Dr. Meghan Azad went back to CHILD’s vast repository of biological samples and began looking closely at individual breastmilk components.
With Dr. Shirin Moossavi, a former PhD student and now a 2020 Canadian Institutes for Health Research (CIHR) Postdoctoral Fellow (University of Calgary), the researchers focused in on the bacteria contained in breastmilk,
“We saw that it was highly variable – milk from different mothers contained different types and combinations of bacteria,” says Dr. Moossavi. “So, our next question was, why the differences?”
Using information collected from the mothers, Drs Azad and Moossavi analyzed factors that might influence the milk bacteria. They considered whether the mother delivered vaginally or by C-section; her weight, age, diet, and ethnicity; and breastfeeding practices, such as exclusivity, duration and the method of feeding.
They discovered that milk bacteria were different in mothers who pumped their milk, compared to those who fed their infant directly from the breast.
In fact, of all the variables they analyzed, breastmilk pumping was the one factor consistently associated with differences in milk bacteria.
“This may offer us a clue as to why babies who consume pumped breast milk are at greater risk of asthma, allergies and early obesity than those who feed straight from the breast,” says Dr. Moossavi.
BREASTMILK BACKWASH?
How to explain the results? Drs Azad and Moossavi suspect that pumping may prevent the transfer of bacteria from the infant’s mouth to the mother – in other words, when a baby is nursed, the baby’s saliva can creep back into mom’s nipple, and “this transfer may be prevented if the baby is fed from a bottle,” explains Dr. Moossavi.
Pumping might also introduce other bacteria from the pump itself, which could alter the bacterial profile in mom’s milk.
The research was published in the journal Cell Host & Microbe and was one of the journal’s most cited papers in 2019.
The paper also drew a lot of interest from mainstream media, including from CBC’s Quirks and Quarks.
As often happens in translating research for the public, however; “some reports exaggerated the implications of the study and cast pumping in a somewhat negative light,” says Dr. Azad.
“But that’s not what people should conclude from our research. Pumped breastmilk gives baby many of the same health benefits as nursing – it’s just that nursing may have a slight edge – and we want to understand why, in order to provide helpful advice to moms who pump.”
Mom and baby share “good” bacteria through breastmilk
test
Dr. Meghan Azad’s research into the profile of breastmilk bacteria in Cell Host & Microbe in 2019 prompted several more intriguing research questions, such as: Is a mom’s breastmilk bacteria shared with her baby? If so, how does it get there?
There was one way to find out: by comparing the bacteria in mom’s breastmilk to the bacteria in her infant’s gut. CHILD researchers had already profiled each baby’s gut bacteria from stool collected in the diaper, “so it was just a question of looking at the bacteria in the breastmilk and connecting the dots,” says Dr. Azad.
For the analysis, Drs Azad and Shirin Moossavi teamed up with CHILD colleagues Dr. B. Brett Finlay and Dr. Stuart Turvey (The University of British Columbia). Together, they found that a mother’s breastmilk and her infant’s gut microbiome shared some of the same bacteria, including bacteria that previous CHILD research by Drs Finlay and Turvey found to protect against asthmatic wheeze.
PROTECTIVE BACTERIA
“It’s not just nutrients and immune components that moms transfer to their babies through breastmilk; they also seem to transfer ‘good bacteria’ that protect babies from illness and infections,” comments Dr. Azad. “Our study also showed that the co-occurrence of shared ‘good’ bacteria was higher when infants nursed directly at the breast.”
Published in Cell Host & Microbe in August 2020, Dr. Azad believes that this latest research supports their earlier hypothesis that the process of pumping, storing and bottle-feeding breastmilk may reduce the transfer of viable milk bacteria from mom to baby.
The results also support the idea that breastmilk may act as an incubator that protects and transports certain bacteria to a baby’s intestinal tract.
“This also gives us some idea as to which bacteria could make good probiotics, since they appear to withstand the trip to the baby’s gut,” she adds.

Image from CHILD Cohort Study breastfeeding video
CHILD Cohort Study generates “triple exposure” hypothesis for protection against peanut allergy
test
In late 2020, Dr. Meghan Azad’s breastfeeding research investigated the relationship between maternal peanut consumption, breastfeeding, and infant peanut consumption in the development of peanut sensitization – an early sign of allergy risk.
“There is now ample evidence that early peanut introduction helps to reduce a child’s risk of developing peanut allergy, and infant feeding recommendations have been updated to reflect this over the last few years,” says Dr. Azad.
“As someone who researches breastfeeding, I have been curious about how a mom’s peanut intake might play a role in this scenario, because we know that peanut protein can be transferred through breastmilk.”
PEANUT FOR MOM & BREASTFEEDING BABY: LOWER ALLERGY RISK
Using data from 2,759 moms and infants participating in CHILD, Dr. Azad’s team found that eating peanuts while breastfeeding, combined with introducing peanuts to babies before 12 months of age, may reduce the risk of peanut allergy by age five.
In line with previous research, the study found that infants who were fed peanut before one year of age had a reduced risk of peanut sensitization at age five compared to children who did not consume peanut in their first 12 months.
The difference was substantial (66% reduced risk) for infants if they were not breastfeeding at the time of peanut introduction, but it was greater still (88% reduced risk) when mothers introduced peanut early while breastfeeding and regularly consuming peanut themselves.
“We call it the ‘triple exposure hypothesis,’” Dr. Azad explains.
“We did not see a direct beneficial association for breastfeeding alone in relation to peanut sensitization. However, if a mom breastfed, ate peanut herself and introduced it early to her child, the combined effect of all three exposures seemed to offer an enhanced protection against peanut sensitization and future allergy risk.”
The study was published in the Journal of Developmental Origins of Health and Disease in December 2020.
GROWING EVIDENCE FOR EARLY INTRODUCTION
Dr. Malcolm Sears (McMaster University), the founding Director of CHILD and a study co-author, says these findings build upon a growing body of evidence from CHILD about the importance of introducing potentially allergenic foods early.
While further studies are needed, the authors believe the current findings support guidelines recommending early peanut introduction for allergy prevention and contribute new evidence that maternal peanut consumption and breastfeeding could further enhance this protective effect.
“We hope that this research may also eventually contribute to the development of supplements or therapeutics for mothers who cannot safely consume peanut, and for infants who cannot be breastfed,” says Dr. Azad.
Gates Foundation grant a “game-changer” for breastmilk research
test
In February 2020, Dr. Meghan Azad received a $6.5 million grant from the Bill & Melinda Gates Foundation to lead a new global health initiative dedicated to breastmilk.
As Director of the new International Milk Composition (IMiC) Consortium, Dr. Azad will bring together five research groups studying maternal nutrition and infant growth in Tanzania, Pakistan, Nepal, Burkina Faso and Canada. The consortium will study global differences in breastmilk and establish a biorepository of human milk samples.
STUDYING MILK & RESILIANCE
During the next three years, IMiC researchers will analyze samples of breast milk from 1,200 mother-infant pairs.

Their aim is to understand the components of human milk that influence infant growth and resilience in order to inform nutrition recommendations and interventions for moms and babies.
CHILD WORK ATTRACTS ATTENTION
Dr. Azad said it was her breastfeeding research within CHILD that first attracted representatives from the Gates Foundation to consider her for the funding.
“At a nutrition conference, I presented my CHILD results showing an association between breastfeeding and health outcomes such as asthma and obesity, and members of the Gates Foundation approached me afterwards to learn more,” she says.
While IMiC is a global initiative, the grant will allow Dr. Azad to continue analyzing the breastmilk samples collected in CHILD, with the goal of uncovering the role of maternal nutrition, infant feeding and human milk composition in the development and prevention of asthma, allergies, obesity and diabetes.
Watch the CBC interview with Dr. Azad | Read the UM Today article
CHILD’s KT video: Spreading the word about breastfeeding
test
In June 2020, CHILD launched its newest knowledge translation video to share the study’s exciting discoveries about the role of breastmilk in child health and development.
Developed with CHILD stakeholders and study participants to ensure its accessibility and appeal to a wide lay audience, the video was widely promoted by AllerGen and CHILD partner organizations, including the Canadian Institutes of Health Research (CIHR), Asthma Canada, The Sandbox Project, the Canadian Society of Allergy and Clinical Immunology (CSACI), Food Allergy Canada, the Canadian Urban Environmental Health Research Consortium (CANUE), and many more.
In its first month, the video registered over 8,000 YouTube views from viewers in 17 countries as far away as India, Russia and Finland.
After five months, the video had acquired over 16,000 views and received international requests for translation.
The video is now available with Japanese, Vietnamese and Chinese subtitles, and can also be viewed with the main title and video description translated to several additional languages.
Mothers who consume more fruit while pregnant may give their babies a brain boost
test
Research from AllerGen’s CHILD Cohort Study (CHILD) suggests that children may reap the health benefits of fruit even before birth.
Dr. Piush Mandhane (University of Alberta), leader of CHILD’s Edmonton site, analyzed data from nearly 700 mothers and children involved in CHILD, and found that mothers who consumed more fruit during pregnancy gave birth to children who performed better on developmental testing at one year of age.
“We wanted to know if we could identify prenatal and postnatal factors that affect cognitive development,” says Dr. Mandhane.
“We found that one of the biggest predictors was how much fruit a mother consumed during pregnancy.”
SUBSTANTIAL DIFFERENCE
Babies born to mothers who consumed six or more servings of fruit per day during pregnancy scored six or seven points higher on an infant development scale at age one compared to babies whose mothers ate less than one serving of fruit.
“It’s quite a substantial difference – that’s half of a standard deviation,” notes Dr. Mandhane.
The research team also looked into the specific nutrients the mothers consumed as part of their fruit intake. Two “stars” emerged: lycopene – a natural pigment that gives fruits and vegetables, such as tomatoes, grapefruit and watermelon their red colour – and fructose, the natural sugar found in most fruit and vegetables.
JUICE DOESN’T DO IT
Published in EBioMedicine in June 2016, the research puts a new spin on nutrition during pregnancy: the results suggest that it’s not just the nutrients that count, but their source.
“Fruit juice did not have the same beneficial effect on infant development,” says Dr. Mandhane, “nor did prenatal consumption of vegetables.”
The gestational age of the child at birth also highlighted the effect: the earlier a child was born, the more obvious the “fruit factor.”
In women who gave birth to preterm children, “having one extra serving of fruit per day gave the baby the same benefit as being born a whole week later,” Dr. Mandhane explains. “That’s a meaningful advantage.”
National and international news outlets, including CBC, Good Housekeeping, The Wall Street Journal, and the UK’s The Telegraph, reported the findings.
While the results suggest the more fruit the better, the researchers caution that their study did not consider potential complications of increasing natural sugar intake, such as gestational diabetes and high birthweight.
WORKS WITH FLY BABIES,TOO
To further build on the CHILD discovery, Dr. Mandhane collaborated with Dr. Francois Bolduc (University of Alberta), who showed that flies born after being fed increased prenatal fruit had significantly better memory ability, similar to the results shown by Dr. Mandhane with one-year-old infants.
The researchers believe that this finding suggests that brain function affected by fruit and the mechanisms involved have been maintained through evolution and conserved across species.
“Our future research will investigate whether the benefits of prenatal fruit consumption persist in children over time,” says Dr. Mandhane.
“At age three, we can test a child’s higher cognitive functions like planning and multitasking.”
If prenatal fruit boosts these functions, “there may be a real benefit to promoting greater fruit intake during pregnancy, particularly if we can improve outcomes for premature babies, who are at higher risk of intellectual delays.”
Protein in saliva is related to human stress
test
In November 2020, AllerGen researchers from the University of Alberta received a US patent to develop and commercialize a non-invasive saliva-based test that may ultimately predict, diagnose and help to treat stress-related conditions.
The patent is related to a body of AllerGen-supported research led by Dr. Dean Befus (University of Alberta), co-lead of the Network’s Biomarkers & Bioinformatics Enabling Platform.
Dr. Befus’ research team discovered that a salivary protein called calcium-binding protein spermatid-specific 1 (CABS1) has the potential to be a reliable, accurate marker of human stress.
What’s more, levels of CABS1 may change depending on the kinds of stress we experience.
The protein, which was previously only identified in the male reproductive system, “is a marker of acute psychological stress and feelings of negative mood or emotional distress,” according to Dr. Befus.
“Ultimately, these findings may lead to new ways to predict, diagnose and eventually treat stress-related conditions,” he says.
STRESSED-OUT STUDENTS
In a series of AllerGen-supported studies, Dr. Befus’ team collaborated with psychologist Dr. Thomas Ritz (Southern Methodist University; Dallas, Texas) to conduct stress experiments on university student volunteers. Both immediate (acute) and prolonged (chronic) psychological stress were measured.
In the first study, researchers measured baseline CABS1 concentrations in participants’ saliva over a five-week period.
In the second study, designed to mimic acute stress, student volunteers were given five minutes to prepare an important speech designed to obtain a senior position at a major company. After delivering their speeches, participants were assigned an unexpected and challenging mental arithmetic test.
Researchers collected saliva from participants throughout the experiment.
In the third study, designed to mimic chronic stress, researchers collected saliva from participants during the middle of the university term (a low stress point) and during final exams at the end of the academic term (a high stress point).
The researchers then analyzed the presence of CABS1 in saliva and checked for associations between levels of CABS1 and the participants’ responses to questions about their mood, anxiety, stress and depression across the three studies.
PROTEINS ASSOCIATED WITH STRESS
“In all three studies reported in our paper, there was a connection between stress and the presence of CABS1 in saliva,” says Eduardo Reyes-Serratos, a former AllerGen trainee and first author of the scientific paper published in The American Journal of Physiology in June 2017.
Specifically, levels of CABS1 were increased in the saliva of those participants who self-reported negative mood and acute stress, and of those with higher depressive and anxious mood in the preceding week.
“CABS1 was also associated with markers of inflammatory activity and certain variants of CABS1 appeared to be markers of resilience to stress in some individuals,” says Reyes-Serratos.
With a decade of AllerGen research support behind him, Dr. Befus filed an Intellectual Property (IP) disclosure for the CABS1 discovery in 2016, attracted $50,000 in partner cash and in-kind contributions, and received full patent protection in 2020.
STRESS SCREENING TOOL?
“Given the substantial health and economic burden imposed by stress, we believe a CABS1 saliva-based screening tool could be extremely useful alongside psychological tests to measure an individual’s susceptibility to stress and assist employers in identifying stress-resilient candidates better suited for high-stress occupations,” says Dr. Befus.
How sleep affects an infant’s cognitive and language skills
test
Does your child sleep less than 12 hours over a 24-hour period? Does he or she breathe through the mouth, snore or have pauses in breathing while asleep?
If the answer to either question is yes, findings from the CHILD Cohort Study (CHILD) explain how sleep disruption may affect health, learning and behaviour in young children.
In a pair of studies by Dr. Piush Mandhane (University of Alberta), lead of CHILD’s Edmonton site, CHILD researchers examined the impact of an infant’s sleep duration and disruption due to sleep-disordered breathing (SDB) on cognitive and language development at two years of age, and identified four distinct types of SDB that occur in infants, along with unique risk factors associated with each.
LESS SLEEP, POORER DEVELOPMENT
In the first study, published in Sleep Medicine, Dr. Mandhane’s team found that infants who regularly sleep less than 12 hours total over any given 24-hour period have poorer cognitive and language development at two years of age than infants who get more sleep.
They also found that nighttime sleep had a greater impact on cognitive and language development compared to daytime sleep, and a short nighttime sleep was associated with a 10.1-point decrease in cognitive development using a standardized test of mental and motor development.
“A drop of 10 points represents nearly a full standard deviation on the cognitive scale,” explains Dr. Mandhane. “It’s quite a substantial difference.”
The researchers further found that children with persistent SDB had lower language scores, but no differences in cognitive development compared to children with no SDB.
There are a few possible explanations for this finding, according to Dr. Mandhane. “One theory is that language acquisition is more sensitive to sleep disruption than cognitive development,” he says.
“Alternatively, the link between SDB and language delay may be the result of kids having multiple nose and ear infections, which tend to impair hearing and speech.”
SNORING VARIATIONS
In the second study, the researchers delved into the children’s snoring patterns, hoping to find out if there were different types of snorers and what factors might be influencing them.
They identified four patterns of SDB from infancy to two years of age: i) no SDB; ii) early-onset SDB with peak symptoms at nine months of age; iii) late-onset SDB with peak symptoms at 18 months of age; and iv) persistent SDB with symptoms from three to 24 months.
Infants given acid reflux medication were more likely to have early-onset SDB, while children who were exposed to smoke or dogs in the home were more likely to develop late-onset SDB, the study found.
“We also found that children at risk for allergies or with divorced parents were more likely to present with persistent SDB,” comments Dr. Mandhane.
THE IMPORTANCE OF SLEEP
“Together, these findings highlight the importance of total and nighttime sleep, and demonstrate the cognitive and language problems that can occur in preschool children when sleep is disrupted,” Dr. Mandhane says.
“Our results suggest that early intervention to reduce specific SDB risk factors may help to avoid more serious behavioural, cognitive and emotional problems down the road.”
Mom’s depression in pregnancy affects baby’s immune system
test
UNICEF Canada, the world’s leading child-focused humanitarian organization, featured CHILD Cohort Study (CHILD) results about maternal depression in its April 2018 campaign to improve parental leave policies in Canada.
The CHILD research was led by AllerGen investigator Dr. Anita Kozyrskyj (University of Alberta) and published in November 2017 in Brain, Behavior and Immunity.
STRESS INCREASES ALLERGY RISK
It found that infants born to mothers experiencing psychological distress (stress, depression, anxiety) had reduced levels of an important immune antibody in their feces in the first few months of life, which may put them at a higher risk of developing allergic disease.
The findings, which suggest that programs and policies to support the psychosocial wellbeing of mothers during and after pregnancy are important in shaping the immune health of newborns, were leveraged by UNICEF.
INFORMING POLICY
“CHILD Study research is helping to inform UNICEF’s efforts to advocate for better child and family policies, including improved parental leave take-up that will help more mothers continue breastfeeding and keep more babies healthy”, says Lisa Wolff, UNICEF’S Director of Policy and Research.
For the study, Dr. Kozyrskyj’s team analyzed data from 403 infants and their mothers participating in CHILD.
“We found that when mothers were depressed during and after pregnancy, their infants were more likely to have reduced concentrations of secretory immunoglobulin A (sIgA), a critical immune antibody, in their gut as compared to infants whose mothers were not depressed,” says Dr. Kozyrskyj.
The sIgA antibody is thought to play a critical role in reducing the risk of allergic disease by helping an infant’s developing immune system to recognize the difference between harmful and harmless substances in the gut.
STRESS INDEPENDENT FROM BREASTFEEDING
Because sIgA is passed from moms to infants through breastmilk, the researchers also examined the impact of breastfeeding on sIgA levels.
“We wondered if maternal distress affected breastfeeding, which might explain the lower sIgA levels seen in some infants,” says former AllerGen trainee and study first-author Liane Kang, who is currently a medical student at the University of Alberta.
“However, we found that even with exclusive breastfeeding, infants of mothers with prenatal depression had slightly lower sIgA concentrations, and infants of mothers with both pre- and post-natal depression were three times as likely to have reduced fecal sIgA levels, which suggests that maternal distress is associated with infant sIgA levels, independent of breastfeeding.”
These findings, and other CHILD discoveries, are being taken up by stakeholders such as UNICEF Canada who can put them into practice to improve maternal and child health.
How much screen time is too much for young children?
test
The amount of time young children spend sitting in front of screens has increased with the growing use of gaming consoles and mobile devices.
Recently, restrictions on everyday activities during the coronavirus pandemic have meant that many parents have turned to television, tablets and video games to entertain their kids more than they typically would.
Parents, healthcare providers and educators may be left wondering: How much screen time is too much?
In 2019, the CHILD Cohort Study (CHILD) undertook the largest investigation in Canada to look at screen time exposure among toddlers and preschoolers and to measure its impact on behavioural and emotional problems.
MEASURING IMPACT
Using data from more than 2,400 CHILD Study participating families across Canada, Dr. Piush Mandhane (University of Alberta) and his team found that among preschoolers, two hours or more of screen time per day was linked to clinically significant behavioural problems.
The research was published in the journal PLOS One in April 2019.
Compared with children who had less than 30 minutes per day of screen time, children who were in front of screens for more than two hours were five times more likely to exhibit clinically significant “externalizing” behavioural problems such as inattention and aggression.
They were also more than seven times more likely to meet the criteria for attention deficit hyperactivity disorder.
“There wasn’t a lot of research out there looking at screen time in preschoolers,” says Dr. Mandhane.
“In CHILD, parents had provided detailed information about their children’s activities and screen time use at various ages, and they had also completed a 99-item checklist about their child’s behaviour at age five, covering everything from aggressive behaviour to social withdrawal to sleep. We used this incredible data to analyze the impact of screen time exposure.”
KIDS EXCEEDING RECOMMENDED LIMITS
The researchers found that, on average, three-year-old children spent 1.5 hours a day in front of a screen, while five-year-olds spent an average of 1.4 hours a day. For both ages, the average daily screen time use exceeded Canada’s 24-Hour Movement Guidelines.
“Among the younger kids, 42% of three-year-olds exceeded the recommendation of less than one hour of screen time per day. For five-year-olds, 13% of the children exceeded the recommendation of less than two hours of screen time per day,” reports Dr. Sukhpreet Tamana (Simon Fraser University), first author of the PLOS One paper.
“The two big takeaways from this study are that children exposed to more screen time, at either age three or five years, showed significantly greater behavioural and attention problems at age five, and that this association was greater than any other risk factor we assessed, including sleep, parenting stress, and socioeconomic factors,” adds Dr. Tamana.

Dr. Sukhpreet Tamana (L) and Dr. Piush Mandhane (back) with CHILD participants in Edmonton, AB
ORGANIZED SPORTS HELP
The researchers also looked for protective factors that made behavioural problems less likely. They found that more than two hours a week of physical activity significantly reduced children’s risk of behavioural problems at age five.
Good quality sleep had a small impact and participation in organized sports was found to have a highly significant protective effect.
“Interestingly, it wasn’t physical activity on its own that was protective; the activity needed to have structure,” Dr. Mandhane explains. “And the more time children spent doing organized sports, the less likely they were to exhibit behavioural problems.”
The research made a splash in the mainstream media. From CBC News and The Globe and Mail to People.com and Newsweek, major news outlets picked up the story and invited Drs Mandhane and Tamana to comment on their findings.
Dr. Mandhane continues to follow the CHILD cohort of children as they grow up, to see if the association between screen time and behaviour persists over the years.
MODERATION, VARIED ROUTINES ARE BEST
In the meantime, he recommends that screen time be limited to less than two hours a day for young children and he regards the preschool years as “the ideal time to promote healthy relationships with screens.”
And what to do during the pandemic, when restrictions on activities have brought many children closer to screens than ever?
“Parents should not feel guilty during this time,” Dr. Tamana offers. Instead, “We suggest that they set up a routine that breaks up the screen time with activities such as indoor and outdoor play, arts and crafts, games, or quiet-time activities such as reading or story time.”
CHILD Cohort Study receives major funding to study the infant microbiome
test
From our skin to each of our organs, the human microbiome – the trillions of microbes and bacteria that live on and in our bodies – impacts our health and well-being, and can influence the development of disease.
The CHILD Cohort Study is a unique Canadian research project studying the microbiome, and the health and development of 3,500 children across the country from pregnancy to school age and beyond.
By following these children (and their families) over many years, CHILD has made exciting discoveries about how the types and balance of certain bacteria can shape health, and how changes to the microbiome may partly explain the shifting rates of childhood asthma, allergies, obesity and other chronic diseases.
In 2018 and 2020, CHILD received two major federal grants to further advance the Study’s groundbreaking microbiome research.
GRANT 1: ASTHMA PREDICTION
In the first grant, CHILD researchers received over $9 million to look for a way to predict which babies will go on to have asthma, based on the infant’s microbiome.
CHILD’s Co-Director Dr. Stuart Turvey (University of British Columbia) heads the four-year project. Dr. Turvey and other members of the project team have previously shown that babies lacking certain microbes in their gut tend to develop asthma.
They will now use powerful new genomic technologies to catalogue the gut microbes associated with asthma – particularly the ‘missing’ microbes in infants who later develop asthma – and to develop a screening tool to identify infants at the highest risk of asthma.
This, in turn, may enable the development of new strategies to prevent asthma from developing in the first place.
The $4.5 million in funding from Genome Canada, combined with contributions from the Canadian Institutes of Health Research (CIHR) and other partners to total $9.1 million, was announced on January 23, 2018, by federal Science Minister the Honourable Kirsty Duncan.
GRANT 2: ROLE OF MICROBIOME IN HEALTH & DISEASE
The second grant, announced in January 2020, funds a five-year, $2 million project co-led by CHILD Director Dr. Padmaja Subbarao (The Hospital for Sick Children) and CHILD’s Manitoba site co-lead Dr. Meghan Azad (University of Manitoba).
Funding was announced by the Honourable Patty Hajdu, Canada’s Minister of Health, as part of an $18-million investment from the Canadian Institutes of Health Research (CIHR) to better understand the role of the microbiome in human health and disease through the Canadian Microbiome Initiative 2 (CMI2) program.
The project will mine the extensive environmental, clinical and microbiome data, and biological samples available from CHILD to investigate:
- how an infant’s genetics, sex, and early-life exposures influence the microbiome-immune system co-development;
- the importance of breastmilk and antibiotics in shaping the infant gut microbiome;
- the impact of the microbiome on the risk of asthma; and
- microbiome-targeted interventions for asthma in mice.
“Both of these awards will help us further our understanding of the microbiome, which, in turn, will lead to the development of new preventative and therapeutic interventions for asthma,” says Dr. Subbarao.
“These investments signify the incredible value of CHILD as a platform for novel research that can ultimately help to improve the lives of Canadian children.”

CHILD Director Dr. Padmaja Subbarao (left) with Science Minister Kirsty Duncan at the Ministerial announcement in Toronto on January 23, 2018.